Free Michigan Molina Prior Authorization Template in PDF
The Michigan Molina Prior Authorization form serves as a critical tool for healthcare providers seeking approval for various medical services and treatments under Molina Healthcare. This form is designed to streamline the process for obtaining necessary authorizations, whether for Medicaid or Medicare members. It requires essential information, including the member's name, ID number, and contact details, along with specifics about the requested service type—be it inpatient, outpatient, surgical procedures, or home health care. The distinction between elective and urgent requests is crucial; urgent requests must meet strict criteria to prevent serious health deterioration. Providers must also include diagnosis and procedure codes, as well as the number of visits requested and relevant dates of service. Additionally, the form mandates the submission of clinical notes and supporting documentation to facilitate the review process. Clear communication is key, as the form includes sections for both member and provider information, ensuring that all necessary parties are informed and involved in the authorization process.
Form Example
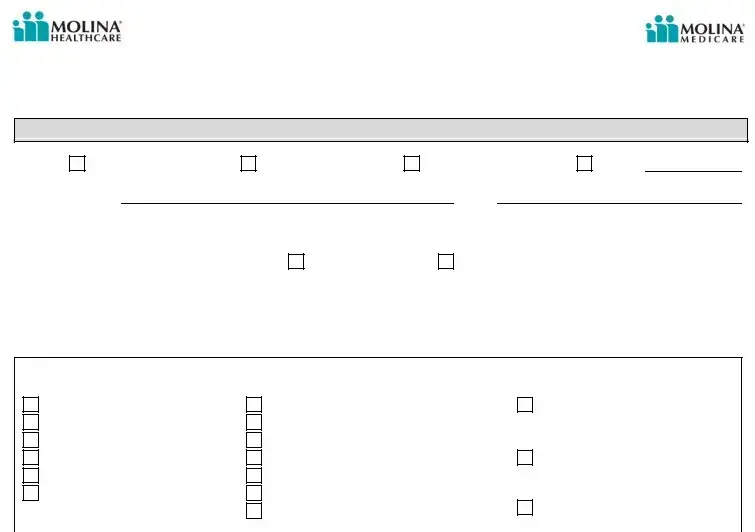
Molina Healthcare of Michigan Prior Authorization Request Form
Phone Number: (888)
Medicaid Fax Number: (800)
Medicare Fax: (888)
Member I nformat ion
Plan: |
Molina Medicaid |
Member Name:
Molina MI Child
Molina Medicare
DOB:
Other:
Member I D# : |
|
Member Phone # : |
( |
) |
Service I s:
Elective/ Routine
Expedited/ Urgent *
*Definition of Urgent / Expedited service request designation is w hen the treat ment requested is required to prevent serious deterioration in the member’s health or could jeopardize the member’s ability to regain maximum function. Requests outside of this definition should be submitted as routine/ non- urgent.
Referral/ Service Type Request ed
|
I npatient |
|
|
|
|
|
|
Outpatient |
|
|
|
||||||
|
Surgical Procedures |
|
|
|
|
|
|
Surgical Procedure |
|
DME |
|
||||||
|
ED Admission |
|
|
|
|
|
|
Rehab (PT, OT, & ST) |
|
|
|
||||||
|
Direct Admission |
|
|
|
|
|
|
Diagnostic Procedure |
|
|
|
||||||
|
SNF |
|
|
|
|
|
|
I maging |
|
Home Health |
|
||||||
|
Rehab |
|
|
|
|
|
|
Chiropractic |
|
|
|
||||||
|
LTAC |
|
|
|
|
|
|
Wound Care |
|
|
|
||||||
|
|
|
|
|
|
|
|
|
I nfusion Therapy |
|
I n Office |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Referred To Provider/ Facility Name & Tax I D# : _____ |
|
|
|
|||||||||||||
|
Referred To Address & Phone# : |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Diagnosis Code & Description: |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
CPT/ HCPCS Code & Description: |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Number of visits requested: |
|
|
|
|
|
Date(s) of Service: |
|
|
|
|||||||
|
|
Please send clinical not es and any support ing document at ion |
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
Provider I nformat ion |
|
|
|
||||
|
Requesting Provider Name and Address: |
|
|
|
|||||||||||||
|
Contact @ Requesting Provider’s: |
|
|
|
|
|
|
|
|
|
|
||||||
|
Phone Number: ( |
) |
|
|
|
|
|
|
|
|
Fax Number: ( |
) |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
For Molina Use Only: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2013 MI Molina Healthcare/ Molina Medicare PA GUI DE 5/ 8/ 13
Document Specs
| Fact Name | Description |
|---|---|
| Contact Information | The Molina Healthcare of Michigan Prior Authorization form includes a phone number: (888) 898-7969. Fax numbers are also provided for Medicaid and Medicare submissions. |
| Member Information | Members must provide their plan type, name, date of birth, ID number, and phone number on the form. |
| Service Type | Requests can be made for various service types, including inpatient, outpatient, surgical procedures, and home health services. |
| Urgent vs. Routine | The form distinguishes between urgent and routine requests. Urgent requests are for services that prevent serious health deterioration. |
| Provider Information | Requesting providers must include their name, address, phone number, and fax number on the form. |
| Diagnosis and Procedure Codes | Providers need to fill in the diagnosis code and description, as well as the CPT/HCPCS code and description for the requested service. |
| Supporting Documentation | Clinical notes and any supporting documents must be sent along with the prior authorization request for review. |
Fill out Common Templates
Michigan Sales Tax Rules - Key for companies to record their economic presence in Michigan, affecting their tax reporting obligations.
The completion of the Texas Homeschool Letter of Intent form is essential for families aiming to educate their children at home, as it officially communicates their intent to the state of Texas. By understanding the requirements outlined in this document, parents can ensure compliance with state regulations and ease the start of their homeschooling journey. For more information, you can visit https://hsintentletter.com/texas-homeschool-letter-of-intent-form/.
How Much Are Closing Costs in Michigan - Exemptions under PA 330 of 1993 are pivotal for refund requests, with the amount requested and the state exemption being claimed clearly indicated on the form.
Michigan Sworn Statement - Contractors use the sworn statement to affirm their financial dealings with subcontractors and suppliers, ensuring all dues are either cleared or accurately reported as outstanding.